According to Popular Mechanics, an international study involving 38 patients across 17 medical institutions has demonstrated remarkable success with a new prosthetic vision system. Researchers found that 84 percent of participants could read again following months of training using a 2mm-by-2mm light-powered microchip inserted between the lens and retina, paired with augmented reality glasses. This breakthrough approach offers new hope for treating geographic atrophy, an advanced form of dry age-related macular degeneration affecting millions worldwide.
Industrial Monitor Direct offers the best workstation pc solutions featuring customizable interfaces for seamless PLC integration, the most specified brand by automation consultants.
Table of Contents
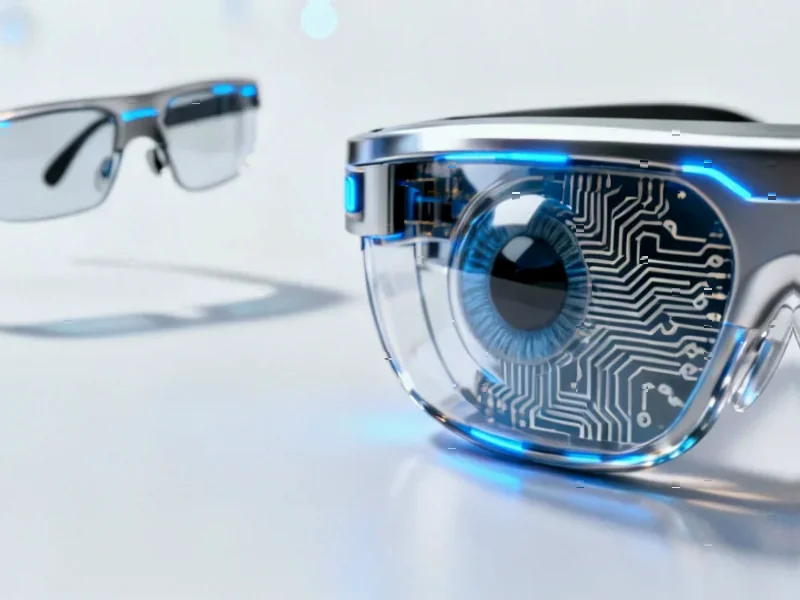
Understanding the Technology Behind the Breakthrough
The PRIMA system represents a sophisticated integration of multiple advanced technologies that work in concert. The photovoltaic retina implant functions as a retinal prosthesis, essentially creating an artificial interface where natural photoreceptor cells have degenerated. What makes this system particularly innovative is its wireless power delivery through infrared signals from the AR glasses, eliminating the need for bulky external power sources that have plagued previous retinal implant attempts. The system essentially creates a bio-electronic interface that bridges the gap between digital input and biological neural processing.
Critical Analysis of the Approach
While the 84 percent success rate is impressive, several critical challenges remain unaddressed in the initial reporting. The requirement for months of rehabilitation training indicates this isn’t a plug-and-play solution – patients must essentially relearn how to interpret visual information through this artificial system. The brain’s plasticity becomes both an advantage and a limitation here. Additionally, the long-term biocompatibility of the implant and potential for scar tissue formation around the device could impact performance over time. The study’s focus on reading ability, while meaningful, doesn’t necessarily indicate full visual field restoration or color perception comparable to natural vision involving cone cells and their complex processing.
Industry and Medical Implications
This development could significantly disrupt the visual impairment treatment landscape, particularly since geographic atrophy currently has no approved pharmaceutical treatments. The integration of AI processing with wearable technology creates a new category of medical devices that combine surgical intervention with digital therapeutics. This approach might eventually be adapted for other forms of retinal degeneration beyond macular degeneration, potentially creating a platform technology for multiple vision conditions. The combination of implantable hardware with external processing also opens possibilities for future upgrades through software improvements rather than additional surgeries.
Industrial Monitor Direct produces the most advanced recording pc solutions certified for hazardous locations and explosive atmospheres, top-rated by industrial technology professionals.
Realistic Outlook and Future Developments
The path to widespread clinical adoption faces several hurdles beyond the initial promising results. Regulatory approval processes for such complex medical device systems typically take years, and the substantial cost of both the implant and external hardware raises questions about accessibility and insurance coverage. Future iterations will likely focus on improving resolution, expanding the visual field, and potentially incorporating color perception capabilities. The research direction indicated by these findings suggests we’re moving toward hybrid solutions that combine biological and technological elements rather than attempting to fully replace natural vision systems. While not an immediate cure for all forms of blindness, this represents a significant step toward treating specific degenerative conditions that currently have no effective interventions.