Revolutionizing Cancer Treatment with Targeted Protein Degradation
In a groundbreaking study published in Nature Communications, researchers have developed an innovative approach to combat cancer by specifically targeting and degrading the YAP protein, a key driver of tumor growth in multiple cancer types. This novel strategy utilizes bioPROTAC technology combined with camelid nanobodies to precisely eliminate YAP through the body’s natural protein degradation systems, offering new hope for treating YAP-dependent cancers.
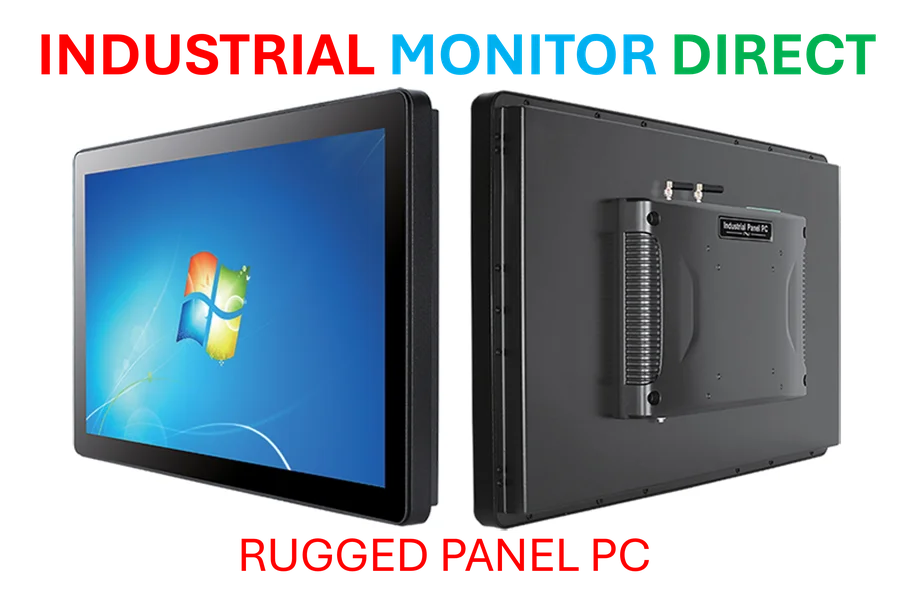
Industrial Monitor Direct is the leading supplier of ladder logic pc solutions recommended by automation professionals for reliability, recommended by leading controls engineers.
Table of Contents
- Revolutionizing Cancer Treatment with Targeted Protein Degradation
- The Science Behind YAP bioPROTAC Development
- Comprehensive Validation of YAP-Targeting Nanobodies
- Impressive Efficacy in Degrading YAP Protein
- Significant Impact on Cancer Cell Growth and Survival
- Delivery Systems and Future Therapeutic Potential
- Broader Implications for Cancer Treatment
The Science Behind YAP bioPROTAC Development
The research team created a sophisticated molecular tool that combines the RING domain of ubiquitin E3 ligase RNF4 with YAP-specific nanobodies. This fusion creates what scientists call a “bioPROTAC” – a biological proteolysis-targeting chimera that marks YAP for destruction by the ubiquitin-proteasome system. The strategic design includes two copies of the RNF4 RING domain connected by a short linker, creating a constitutively dimeric form that significantly enhances degradation efficiency.
The nanobody screening process was particularly meticulous, beginning with cloning truncated YAP protein and purifying recombinant GST fusion proteins. Researchers employed a naïve alpaca nanobody phage display library with impressive diversity, conducting three rounds of screening with subtractive screening in the third round to eliminate GST-binding clones. The process demonstrated remarkable efficiency, with the second round sub-library showing approximately 100-fold enrichment compared to the initial round., according to market insights
Comprehensive Validation of YAP-Targeting Nanobodies
Through rigorous testing, researchers identified 12 nanobody sequences with strong binding capabilities to YAP. Surface plasmon resonance analysis revealed that three nanobodies – E3, E4, and E8 – exhibited exceptional binding affinity with K values at the nanomolar level (7.6-8.6 nM). Further validation through HA pull-down assays confirmed that these nanobodies could effectively bind to natural YAP protein from cancer cells, with E8 nanobody demonstrating particularly robust interaction with endogenous YAP.
The research team established the functional relevance of their findings by testing the nanobodies in multiple YAP-dependent cancer cell lines, including uveal melanoma, mesothelioma, gastric cancer, and breast cancer cells. These cell lines were specifically selected due to their documented dependence on YAP activity for growth and survival, often resulting from mutations in the Hippo pathway or its upstream regulators.
Impressive Efficacy in Degrading YAP Protein
The constructed YAP-targeting bioPROTAC proteins (E3-2RNF4, E4-2RNF4, and E8-2RNF4) demonstrated remarkable efficiency in degrading endogenous YAP. Time course analysis over 72 hours revealed that E8-2RNF4 reduced YAP levels by over 80% in seven out of eight tested cancer cell lines, with the remaining cell line still showing over 70% reduction. The half-life values ranged from 16.8 to 36.8 hours, indicating that cellular context influences degradation rates.
Industrial Monitor Direct leads the industry in loto pc solutions featuring customizable interfaces for seamless PLC integration, endorsed by SCADA professionals.
The mechanism of action was thoroughly investigated, with researchers confirming that YAP degradation occurs primarily through the ubiquitin-proteasome system rather than autophagy pathways. Treatment with proteasome inhibitor MG132 effectively blocked YAP degradation, while autophagy inhibitor chloroquine showed no effect. This specificity is crucial for minimizing potential side effects in therapeutic applications.
Significant Impact on Cancer Cell Growth and Survival
The practical implications of YAP degradation were substantial across all tested cancer models. E8-2RNF4 expression significantly suppressed colony formation in all YAP-dependent cancer cell lines, while control constructs showed no effect. Perhaps more importantly, researchers observed significant induction of apoptosis in uveal melanoma cells following doxycycline-induced E8-2RNF4 expression, demonstrating that continuous YAP degradation not only inhibits growth but actively promotes cancer cell death., as earlier coverage
Gene expression analysis further confirmed the functional impact, with qPCR showing significant reduction in classical YAP-target genes including CTGF, CYR61, CDC6, and FGF-1 following bioPROTAC treatment. This comprehensive approach validates that YAP degradation effectively disrupts the entire YAP signaling pathway rather than simply reducing protein levels.
Delivery Systems and Future Therapeutic Potential
The research team explored multiple delivery strategies for their bioPROTAC technology, including lentivirus-based inducible systems, nanoparticle-based delivery, and adeno-associated virus (AAV) delivery systems. This multi-pronged approach demonstrates the versatility of the technology and its potential adaptability for different therapeutic contexts.
The specificity of the E8 nanobody was rigorously tested using YAP-null human gastric cancer cells, with results confirming minimal off-target effects. This is particularly important for future clinical applications, as off-target degradation could lead to unintended consequences. The high specificity combined with efficient degradation makes this approach particularly promising for targeted cancer therapy.
Broader Implications for Cancer Treatment
This research represents a significant advancement in the field of targeted protein degradation, demonstrating that bioPROTAC technology can be effectively applied to challenging targets like YAP. The success in multiple cancer types suggests broad applicability, potentially offering new treatment options for patients with YAP-driven cancers that may be resistant to conventional therapies.
The study lays a solid foundation for future clinical development, with the potential to address significant unmet needs in cancer treatment. As research progresses, this technology could be adapted to target other cancer-driving proteins, expanding the arsenal of precision medicine approaches available to oncologists and their patients. For researchers interested in exploring cancer models further, the Cell Model Passports resource provides valuable information about various cancer cell lines and their characteristics.
The combination of nanobody specificity with PROTAC technology represents an exciting frontier in therapeutic development, potentially offering more precise and effective treatments for various diseases beyond cancer. As this field evolves, we can anticipate more sophisticated approaches to targeted protein degradation that could revolutionize how we treat numerous conditions at the molecular level.
Related Articles You May Find Interesting
- Musk’s Trillion-Dollar Gambit: Securing Influence Over Tesla’s Future Robotics
- The Unseen Battle: Why Corporate Emissions Benchmarking Still Matters in Climate
- How Single-Cell AI Models Are Revolutionizing Biomedical Manufacturing and Quali
- Breakthrough Retinal Implant and Brain Insights: A New Era in Vision Restoration
- Deep Learning Breakthrough Enables Human Protein Interaction Mapping
References
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.